Nicola Galbraith, senior manager, Gilead HIV Standards Support Team

This article and the ‘Mental well-being and sleep education modules are organized, developed and funded by Gilead Sciences, wwith input from experts in the field of HIV, psychological well-being and sleep.
During my time as an HIV clinical nurse specialist in the NHS, I witnessed the evolution of HIV care from acute in nature to an often manageable, long-term condition. This is testament to the great progress that has been made in the field of HIV and a welcome shift, which comes with a number of new and evolving challenges.
Now that we are working with fellow HIV nurses as part of the Gilead HIV Standards Support Team, we can use our own experiences and insights to shape how the industry can provide valuable, additional support to HIV services.
Recently, in collaboration with clinical and community experts, we developed a series of educational training materials to support healthcare professionals in having conversations about sleep and psychological well-being among people living with HIV.
People living with HIV are disproportionately affected by psychological well-being and sleep problems (Chaponda et al, 2017)
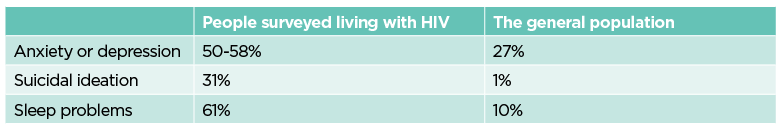
The relationship between HIV, mental health and sleep is closely intertwined (Croston and Rutter, 2020; Warner and Rutter, 2020; BPS, 2019; British HIV Association, 2018; BPS et al, 2011).
A diagnosis of HIV brings unique challenges such as discrimination, isolation and a lack of understanding, all of which can contribute to poor psychological well-being.
Mental health problems can significantly impact a person’s adjustment to their diagnosis, their relationships with healthcare providers, and their adherence to treatment. This in turn can lead to poorly controlled HIV infections and poorer health outcomes.
Furthermore, poor mental health often disrupts sleep patterns and physical well-being, exacerbating psychological problems.
“Recognizing mental health care as a central part of the multidisciplinary HIV team approach is critical to ensuring we can support people living with HIV to achieve the best possible physical and mental health outcomes. We need to equip HIV care providers with the knowledge to screen for mental health problems and support them to provide psychologically informed care and make referrals with confidence.”
Sarah Rutter, Clinical Psychologist and Psychology Lead at North Manchester General Hospital’s HIV Service
There is room for improvement in current mental health and sleep assessments and interventions (Brown et al, 2022)
Recently, our team conducted market research among 39 clinics reporting on data from 665 people living with HIV. The results clearly indicated that healthcare professionals are experiencing an increasing demand for psychological well-being and mental health support services.
However, the research also revealed significant differences in practice, alongside a lack of guidance, resources and capacity to facilitate the identification, management and ongoing monitoring of psychological wellbeing and sleep (Brown et al, 2022).
The findings indicate that there is a great need for improvements in this area, as continued monitoring and assessment are critical if we are to improve long-term health outcomes and improve the quality of life for people living with HIV.
Healthcare professionals can feel better informed and confident in the support they recommend
To bridge this gap and equip healthcare professionals with the necessary tools, skills, confidence and knowledge, the Gilead HIV Standards Support Team training program provides an overview of existing relevant guidelines, practical strategies for implementing the current standards of clinical practice, and information on common screening tools. , available resources and pathways for referrals regarding psychological issues and sleep problems.
“Without the right training and resources, it is not always possible for healthcare professionals to feel comfortable providing mental health care to people living with HIV. If mental health needs are not met in our patient cohort, this could have detrimental effects on their health, quality of life, and HIV care. Helping healthcare providers understand common mental health issues in HIV populations, the underlying causes of psychological distress, and the variety of supports they can provide is the first step in untangling this complex web. Combined with practical advice on how to screen and provide some emotional support to improve patients’ psychological well-being, these training modules are designed to ensure that mental health is made a priority in HIV care.”
Dr. Shimu Khamlichi, Clinical Psychologist, Royal Free Hospital London
If you would like to find out how you can help advance care in this area, please contact one of our HIV Standards Support Teams about the training modules: HIVStandardsSupport@gilead.com
At Gilead, we believe that together we can end the epidemic for everyone, everywhere.
VK-UNB-4284 | August 2023
References
British HIV Association (2018) Standards of care for people living with HIV. BHIVA.
British Psychological Association (2019) British Psychological Society response to the APPG on HIV and mental health in England. BPD.
British Psychological Society et al (2011) Standards of psychological support for adults with HIV. BHIVA.
Brown A et al (2022) Psychological well-being and sleep in human immunodeficiency virus (HIV): a retrospective analysis of assessment and interventions within HIV services in the UK and Ireland (UKI).
Chaponda M et al (2017) Systematic review of the prevalence of psychiatric conditions and sleep disorders as comorbidities of HIV infection in Great Britain. International journal for STD and AIDS; 29:704-713.
Croston M, Rutter S (2020) Psychological perspectives in HIV care: an interprofessional approach. Routledge.
Warner S, Rutter S (2020) Traumatic Beginnings, Complicated Lives: Attachment Styles, Relationships, and HIV Care. In: Croston M, Rutter S, eds. Psychological perspectives in HIV care: an interprofessional approach. Routledge.
NT Contributor
 Healthy Famz Healthy Family News essential tips for a healthy family. Explore practical advice to keep your family happy and healthy.
Healthy Famz Healthy Family News essential tips for a healthy family. Explore practical advice to keep your family happy and healthy.


